The Risk of Multiple Medications in the Elderly
A Prescription for Health Risk
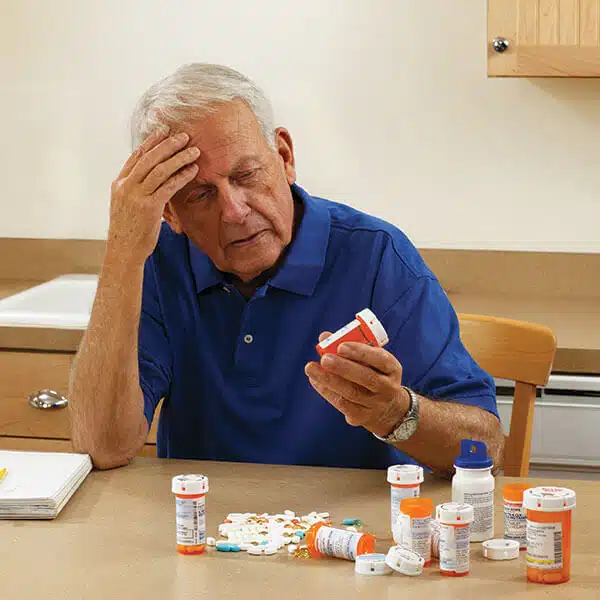
Multiple prescription drug trends are impacting older adults, creating a perfect storm that increases their risk of adverse health outcomes and falls.
Medication use by elderly Canadians has become a hot topic in healthcare circles as studies reveal disturbing trends in multiple drug use, over-prescribing and non-adherence.
This is a troubling development given the proven correlation between polypharmacy and adverse health impacts, including falls.
28% of ER visits are caused by medication problems
More seniors taking more medications
According to the Canadian Institute for Health Information, the proportion of seniors taking multiple medications is rising, with nearly 66% of seniors in public drug programs having claims for 5 or more drugs and nearly 25% having claims for 10 or more medications. A recent University of Toronto study backs this up, stating that the average Canadian senior is now taking an average of seven medications a year.
Multiple medication use has long been proven to correlate with an increase in falls and medical emergencies due to adverse drug interactions and side effects, but the U of T study also shows that each additional medication taken is associated with a 2 – 3% increase in the likelihood of hospitalization and a 3 – 4% increase in the likelihood of an Emergency Room visit.
Over-prescribing inappropriate/high-risk medications
As the number of prescription medications available has increased, so too has the number of medications that are not suited to or carry a high risk for elderly patients. Unfortunately, these medications are too often finding their way into older adults’ medicine cabinets.
Researchers at the University of British Columbia estimate that more than one in three Canadian seniors takes a medication that should be avoided by older patients, a problem they say costs our healthcare system $419 million each year, and as much as $1.8 billion annually once the impact of hospitalizations due to falls and fractures is taken into consideration.
The over-prescribing problem has now reached the point where Canadian healthcare workers, patient groups and governments are working to decrease seniors’ use of high-risk medications by 50% by the year 2020. A Canadian website, deprescribing.org, has also been established to share and exchange information about deprescribing approaches and research with healthcare providers, researchers and the public.
40% seniors over 85 take 10+ pills per day
1 in 3 seniors takes a medication that should be avoided
50%
of patients do not take their medications as prescribed
Non-adherence
Even when older adults are taking safe medications that are medically necessary, there is also an ongoing and significant problem with patients not taking their drugs as prescribed.
It is estimated that as many as 50% of patients do not follow their prescribed regimen, with the elderly being less likely to adhere than average. The reasons why are multifaceted, ranging from the patient’s lack of understanding or acceptance of why their medications are required and how they should be taken to side effects to the cost of the medications and a lack of clear, effective communication between the physician and the patient.
The results of non-adherence are significant, including a 5.4 times increase in the risk of hospitalization, re-hospitalisation and premature death for patients with high blood pressure; a 2.5 times increase in the risk of hospitalization for patients with diabetes; and a more than 40 percent increase in nursing home admissions.
Surprisingly, the rate of medication adherence has not changed in three decades, despite the efforts of numerous health groups including the World Health Organization and the Institute of Medicine.
In our continued efforts to reduce medication non-adherence and prevent the negative medical outcomes that can result, healthcare professionals must take extra care to ensure that we focus on clear, direct communication with our patients and make use of all the tools and resources available to us.
SOURCES
- Health Care in Canada: A Focus on Seniors and Aging, 2011; Canadian Institute for Health Information.
- More is not always better: More drugs mean seniors more likely to land in hospital, says study; National Post, October 11, 2016.
- Allin, S., et al., Does Increased Medication Use among Seniors Increase Risk of Hospitalization and Emergency Department Visits?; Health Services Research, September 27, 2016.
- Harmful medication prescribing to Canadian seniors costs $419M a year; CBC News, June 22, 2016.
- Deprescribing medications for seniors a safety priority; CBC News, February 26, 2016.
- Hoban, Sandra; Falls risks vary with medications, studies find; www.iadvanceseniorcare.com.
- Brown, M. and Bussell, J.; Medication Adherence: WHO Cares?; Mayo Clinic Proceedings, April 2011.
- Medication Adherence – Improving Health Outcomes; American College of Preventive Medicine, 2011.